📘 Table of Contents
- Introduction — What Is Cervical Cancer?
- The Cervix: Anatomy & Function
- What Causes Cervical Cancer?
- Risk Factors: Who Is More Likely to Get It?
- Symptoms & Signs
- Screening and Early Detection
- Diagnosis & Staging
- Treatment Options
- Living with Cervical Cancer
- Prevention Strategies
- Cervical Cancer Awareness & Global Efforts
- Common Questions (FAQs)
- Conclusion
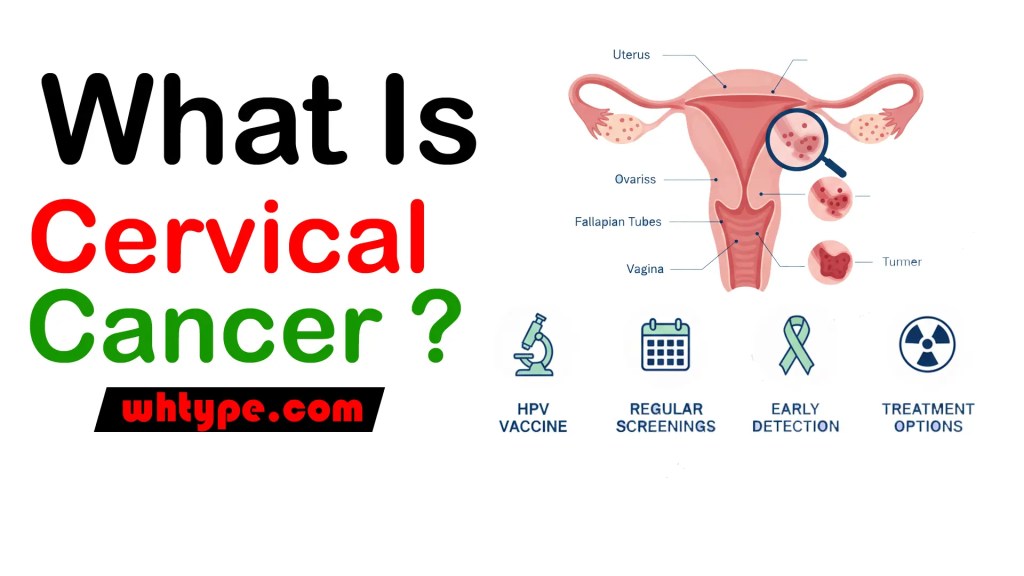
1. 📍 Introduction — What Is Cervical Cancer?
Cervical cancer is a type of cancer that begins in the cervix, which is the lower part of a woman’s uterus (womb) that connects to the vagina. It occurs when normal cells in the cervical lining grow uncontrollably and form a tumour. The condition generally develops slowly over many years and may often start as precancerous changes in cervical cells before evolving into invasive cancer. (World Health Organization)
It is one of the most preventable and treatable cancers when detected early, yet it remains a significant global health problem, especially in areas where regular screening and HPV vaccination are less common. In 2022, around 660,000 women were diagnosed with cervical cancer worldwide, and approximately 350,000 women died from it. (World Health Organization)
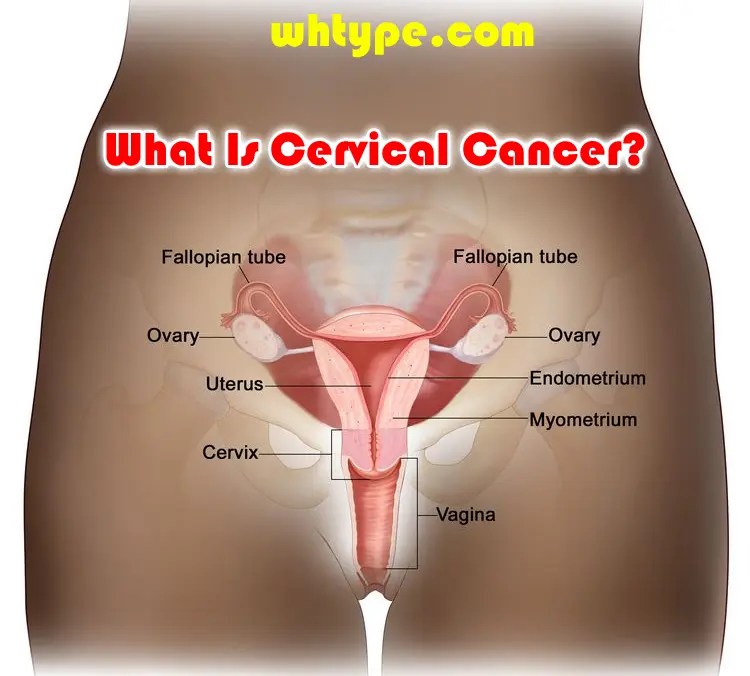
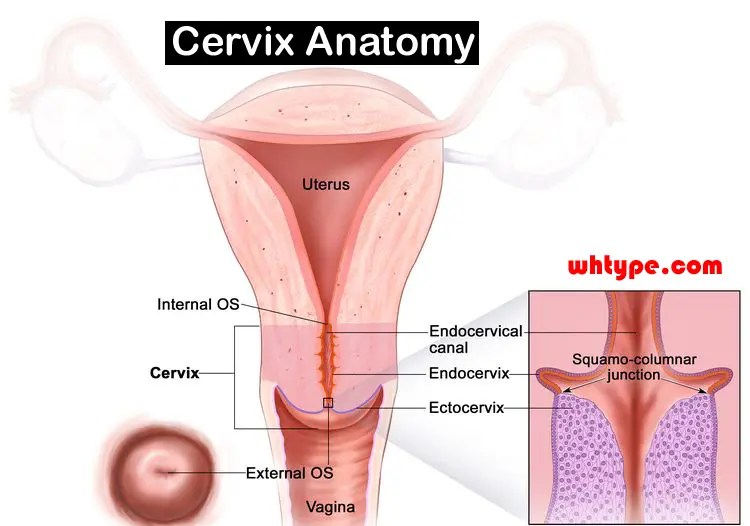
2. 👩⚕️ The Cervix: Anatomy & Function
To understand cervical cancer, it helps to know the cervix’s role in the female reproductive system:
- The cervix is the lower part of the uterus that opens into the vagina.
- It acts as a passageway for menstrual blood, sperm, and childbirth.
- The surface of the cervix is made up of two types of cells — squamous cells (outer surface) and glandular cells (inner canal). Cervical cancer typically begins in these cells.
Cancer arising from the squamous cells is called squamous cell carcinoma, and from the glandular cells is called adenocarcinoma. Both can be detected early with appropriate screening. (Mayo Clinic)
3. 🧬 What Causes Cervical Cancer?
🎯 Primary Cause: Human Papillomavirus (HPV)
Almost all cervical cancers are caused by chronic infection with certain high-risk types of HPV (Human Papillomavirus). HPV is a very common sexually transmitted virus. In most people, the immune system clears HPV naturally, but in some women, the virus persists and causes changes in cervical cells that may eventually lead to cancer. (World Health Organization)
High-risk HPV types — especially HPV-16 and HPV-18 — together account for around 70–80% of cervical cancer cases worldwide. (World Health Organization)
🦠 How HPV Leads to Cancer
- Persistent infection with high-risk HPV over many years damages the DNA in cervical cells.
- Over time, this can cause precancerous lesions (abnormal cell changes).
- Without intervention (through screening and treatment), these changes can become invasive cancer. (World Health Organization)
4. 📊 Risk Factors — Who Is More Likely to Get Cervical Cancer?
Although HPV infection is the main cause, other risk factors increase the likelihood that an HPV infection will persist and develop into cancer:
⏱️ Sexual and Reproductive Factors
- Early sexual activity
- Multiple sexual partners
- Sex with a partner who has many sexual partners
These behaviours raise the chance of HPV exposure and transmission. (www.ndtv.com)
🧪 Lifestyle & Health Factors
- Smoking — Chemicals from cigarette smoke are absorbed into the bloodstream and affect cervical cells, making them more susceptible to HPV-related changes. (Eusuf Memorial Society)
- Weakened immune system, such as from HIV infection or immunosuppressive drugs. (Mayo Clinic)
- Long-term use of oral contraceptives — Some studies suggest a slightly higher risk with prolonged usage. (Eusuf Memorial Society)
⚠️ Other Factors
- Not having regular screening
- Family history of cervical cancer
These factors do not cause cancer directly but can affect risk level and early detection. (World Health Organization)
5. 🚨 Signs & Symptoms of Cervical Cancer
In the early stages, cervical cancer often causes no symptoms at all, which is why screening is critical. Most early cancers are only found through routine Pap tests or HPV testing. (Mayo Clinic)
As the disease progresses, common symptoms may include:
Early Symptoms
- Unusual vaginal bleeding — after sex, between periods, or after menopause. (Cleveland Clinic)
- Unusual discharge from the vagina — watery, bloody, or foul-smelling. (Cleveland Clinic)
- Pain during intercourse (dyspareunia). (Cleveland Clinic)
More Advanced Symptoms
If cancer spreads beyond the cervix, additional symptoms can occur:
- Painful or difficult urination
- Blood in urine or stool
- Pelvic or back pain
- Unintended weight loss and fatigue
These symptoms indicate more advanced disease and require urgent medical evaluation. (Cleveland Clinic)
6. 🧪 Screening and Early Detection
✔️ Why Screening Matters
Routine screening helps detect precancerous changes and early cancers before symptoms appear. Early detection dramatically improves the chances of successful treatment. (MedlinePlus)
📋 Common Screening Tests
- Pap Test (Pap smear):
- Cells are collected from the cervix and examined for abnormalities.
- Can detect abnormal cells before they become cancerous. (Mayo Clinic)
- HPV Test:
- Detects the presence of high-risk HPV DNA in cervical cells.
- Often done together with a Pap test for women over 30. (Mayo Clinic)
🗓️ Recommended Screening Schedule
- Start routine screening at age 21. (Mayo Clinic)
- Women aged 21–29: Pap test every 3 years.
- Women aged 30–65: Pap + HPV testing every 5 years (or Pap alone every 3 years).
- Older than 65: May stop screening if prior tests were normal.
(Schedules may vary by country and individual medical history.) (MedlinePlus)
7. 🔍 Diagnosis & Staging
If screening suggests abnormalities, healthcare providers may do further diagnostic tests:
📌 Colposcopy
- A procedure that uses a special magnifying instrument to closely examine the cervix.
- Allows doctors to see abnormal areas not visible to the naked eye. (Mayo Clinic)
📌 Biopsy
- A small tissue sample is taken from the cervix and examined in a lab to confirm cancer.
- Types include punch biopsy, cone biopsy, or endocervical curettage. (Mayo Clinic)
📌 Staging
Once cancer is confirmed, doctors determine how far it has spread (stage I–IV), which guides treatment strategy. Early stages are usually confined to the cervix or nearby tissues, while advanced stages involve other organs.
8. 🩹 Treatment Options
Treatment depends on the stage of cancer, the patient’s age, overall health, and preferences. Early cancers often have more options and better outcomes.
🔹 Surgery
- Removes cancerous tissue and sometimes reproductive organs.
- Early cancers may be treated with procedures that preserve fertility. (Mayo Clinic)
🔹 Radiation Therapy
- Uses high-energy rays to destroy cancer cells.
- Can be external beam or internal (brachytherapy).
Often used with chemotherapy for advanced cancers. (Eusuf Memorial Society)
🔹 Chemotherapy
- Uses drugs that kill cancer cells throughout the body.
- Often combined with radiation in more advanced stages. (Eusuf Memorial Society)
🔹 Targeted Therapy & Immunotherapy
- Newer treatments that target specific traits of cancer cells or boost the immune system’s ability to fight cancer. (Eusuf Memorial Society)
9. 💪 Living with Cervical Cancer
Coping with a cancer diagnosis involves physical, emotional, and practical challenges. Key areas to focus on include:
✔️ Symptom & Side-Effect Management
- Fatigue, pain, digestive issues, and treatment side effects may occur.
- Supportive care and rehabilitation help manage these symptoms.
✔️ Emotional & Mental Support
- Cancer diagnosis can be stressful and overwhelming.
- Support groups, counselling, and family support improve quality of life.
✔️ Follow-Up Care
- Regular check-ups monitor for recurrence and manage long-term effects.
10. 🛡️ Prevention Strategies
The most effective ways to prevent cervical cancer include:
🧫 HPV Vaccination
Vaccines available protect against high-risk HPV strains responsible for most cervical cancers. WHO recommends vaccination for girls (9–14 years), and some countries include boys too. (World Health Organization)
Recent studies also suggest that even a single dose of HPV vaccine may be highly effective, which could expand access, especially in low-income regions. (AP News)
🩺 Screening
Regular Pap and HPV tests detect abnormalities before they progress to cancer. (MedlinePlus)
💡 Safe Sexual Practices
Using condoms and limiting the number of sexual partners can reduce HPV transmission risk. Condoms don’t eliminate risk entirely but help lower it. (MedlinePlus)
🚭 Avoid Smoking
Smoking weakens immune responses and makes cervical cells more vulnerable to damage. (Eusuf Memorial Society)
🍎 Healthy Lifestyle
A balanced diet, regular exercise, and maintaining immune health support overall disease prevention.
11. 📢 Cervical Cancer Awareness & Global Efforts
Cervical cancer control is a major public health priority. WHO’s Global Strategy to Accelerate the Elimination of Cervical Cancer aims to:
- Achieve 90% HPV vaccination coverage of girls by age 15.
- Ensure 70% of women screened by age 35 and again by age 45.
- Provide 90% access to treatment for women identified with cervical disease. (World Health Organization)
Awareness campaigns worldwide educate women about symptoms, screening, and vaccination. In India, for example, large-scale HPV vaccination drives are underway to reduce the burden of cervical cancer. (The Times of India)
12. ❓ Frequently Asked Questions (FAQs)
1. Is cervical cancer curable?
Yes — when detected early through screening, cervical cancer is often highly treatable and can be cured. (World Health Organization)
2. Can men spread HPV?
Yes — HPV is transmitted through sexual contact by anyone infected, regardless of gender. (World Health Organization)
3. Does HPV always cause cervical cancer?
No — most HPV infections resolve naturally. Only persistent infection with high-risk types can lead to cancer over years. (World Health Organization)
4. At what age is screening recommended?
Screening typically starts at age 21. Talk to your healthcare provider for a personalized plan. (Mayo Clinic)
5. Is the HPV vaccine safe?
Yes — HPV vaccines are safe, with extensive global evidence showing high effectiveness in preventing high-risk HPV infections. (World Health Organization)
13. 🧾 Conclusion — Key Takeaways
- Cervical cancer is largely preventable and treatable if caught early with HPV vaccination and regular screening. (World Health Organization)
- Persistent HPV infection is the main cause, but lifestyle factors and immune status influence risk. (World Health Organization)
- Awareness, access to healthcare, and vaccination programs are essential for controlling this disease globally.
























































































Leave a comment